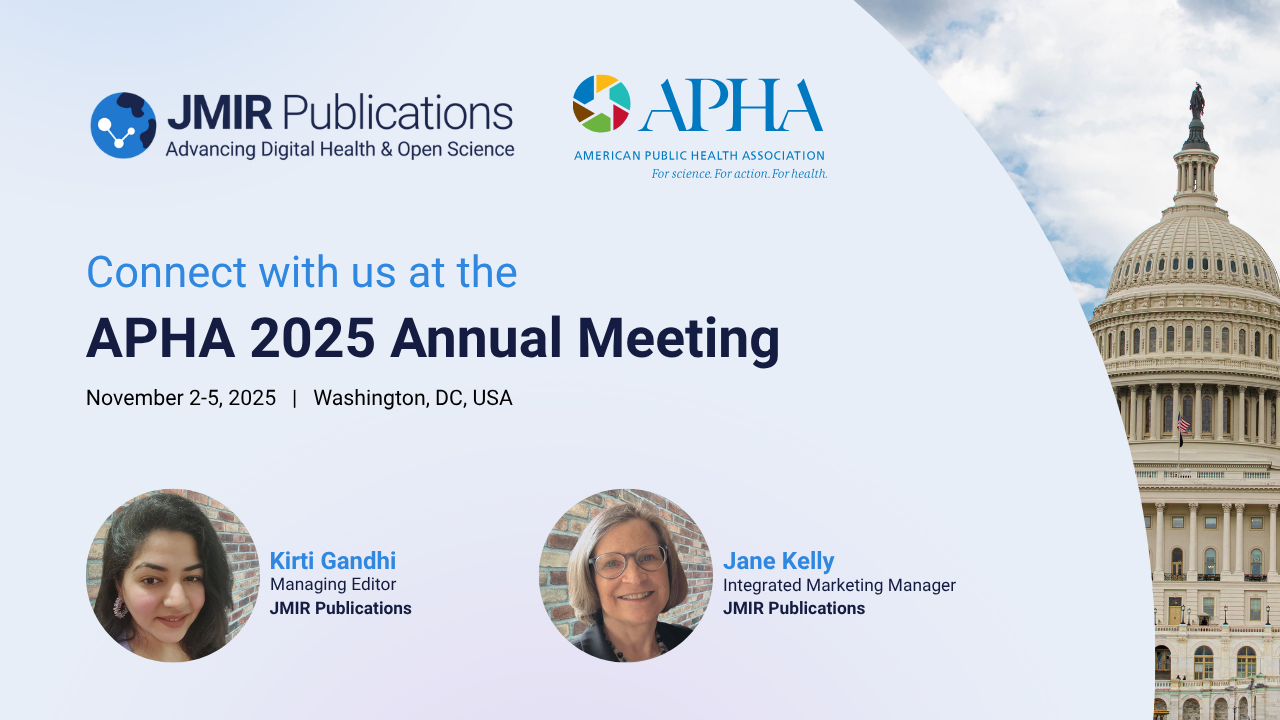
Get Ready, Atlanta! JMIR Publications is Heading to AMIA 2025!
The American Medical Informatics Association (AMIA) 2025 Annual Symposium is fast approaching, and the entire team at JMIR Publications is thrilled to be an exhibitor and active participant!

.png)
.png)




.png)